Best practices in gait rehabilitation
Gait rehabilitation is therapy performed after an injury or illness for the purpose of improving a person’s ability to walk, move around, or balance.
The most common reasons for gait rehabilitation are the onset of a neurological issue (such as stroke, Parkinson’s disease, multiple sclerosis, cerebral palsy, traumatic brain injury, etc.), an orthopedic condition (such hip and knee joint replacement, fractures in the lower limbs, amputation, sports injuries, etc.), medical treatment (chemotherapy, radiation, etc.) or older adults that are experiencing an idiopathic (unknown cause) decrease in their walking ability.

Benefits of gait rehabilitation
There are three significant benefits to gait rehabilitation. The first, and most obvious, is that it provides the client independence and mobility. The second is that it can significantly lower the risk of failing and suffering additional injuries due to instability. The third, if done correctly, is that it can improve cognitive abilities, especially around executive function.
Before getting started with gait rehabilitation, it’s important that the patient and therapist are both comfortable and able to safely do the necessary exercises.
Typical gait training exercises are designed to help strengthen muscles, improve posture and stability, and develop the muscle memory that allows patients to regain their mobility. These activities may include:
- Transfers (like sitting-standing)
- Walking exercise (over ground, treadmill)
- Lifting your legs
- Stepping over objects
- Avoiding obstacles
- Bed exercises
However, clinical trials and the experience of physical therapists strongly indicate that the cognitive exercises are also a critical element in gait rehabilitation. This is driven by the complex interplay between gait and executive function. Better gait improves cognitive function and better cognitive function improves gait.
Best practices for improving gait in older adults
In most people, gait speed begins to decline around the age of 65. This is defined as how quickly one can walk within a specific distance. It also applies to how we walk and move throughout our daily lives.
It is important to recognize that gait speed is a critical physical performance indicator, predicting overall health and life expectancy for people of all ages, but especially for older adults.
Several systems must work together for walking to occur.

Why Does Gait Speed Decline as We Age?
- Poor posture
- Hips and legs become weaker
- Loss of flexibility
- Vision and hearing loss
- Declines in cognitive function
- Dizzy spells and light-headedness
The keys to improving gait speed lies in increasing muscle strength and cognitive functioning.
Spending more time walking is perhaps the most obvious way to increase gait speed. Walking consistently will improve gait speed for most older adults, especially when combined with strength training.
For older adults living in senior communities, walking exercises should be gradually more challenging to improve their skills. Using a virtual reality system such as the GaitBetter technology on a treadmill is a safe and effective way to achieve this. As a result, participants gain the ability to adjust walking patterns easier while using less effort.
Ways to Increase walking challenges and Gait training exercises:
- Adjust speeds for short distances
- Change walking directions
- Add obstacles on the walking path
- Dual tasking while walking
Surgery on the lower extremities, such as the foot, ankle, knee, and hip, can cause a person to experience weakness or tightness in their legs, preventing them from walking normally. Balance and proprioception are also often affected. In most cases, a physical therapist will assess the gait and develop an exercise plan to help improve it.
Exercises often include:
- Choosing the right assistive device
- Range of motion exercises
- Lower extremity strengthening
- Stepping over obstacles
- Target stepping
- Retro walking
- Balance and proprioception exercises
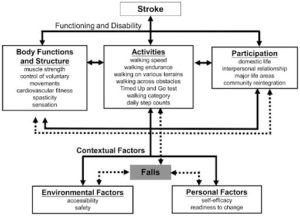
Best practices in gait rehabilitation after stroke
An estimated one in four people will suffer a stroke in their lifetime. Ninety percent of stroke survivors have some functional disability, with degraded mobility being a major and common impairment. As a result, one of the highest priorities of therapists working with post-stroke patients is to quickly improve walking ability to the highest possible outcome.
Being able to confidently walk for extended distances has numerous health benefits for the post-stroke survivor. It reduces social isolation, prevents depression, dramatically lowers the risk of heart disease or osteoporosis, and make it much less likely they will be re-hospitalized due to injuries from falls.
There are a wide range of strategies and assistive devices have been developed to help accelerate gait recovery.
Intervention aims to optimize walking performance by:
- Prevention of adaptive changes in lower limb tissues
- Retraining voluntary response in the lower muscle groups
- Increasing muscle strength and coordination
- Boost walking velocity and endurance
- Develop cardiovascular fitness
- Raising flexibility and balance

The major emphasis in gait training exercises:
- Supporting the body’s mass over the lower limbs
- Increasing momentum of the body’s mass
- Balancing the body’s mass as it moves over one or both lower limbs
- controlling leg movement
- Increase foot clearance
- Accurate foot position and placement
- Optimizing rhythm and coordination
In patients with stroke or similar indications (such as multiple sclerosis), conventional treadmill exercises are frequently used to treat gait disorders. Adding a virtual reality (VR)-based treadmill training can increase motivation and improve therapy outcomes.
Furthermore, the results of a study conducted with the GaitBetter VR treadmill have shown improvements in TUG (Timed Up and Go test), FSST (Four Steps Square Test) and distance walked in 2 minutes walk test, after 5 weeks of training.
Virtual reality rehabilitation system

It is crucial to strengthen the mind-body connection during gait rehabilitation exercises in order to increase brain plasticity and the body’s capability to send signals between the brain and muscles.
Adding a virtual reality element to treadmill training is proving to be a beneficial step in gait rehabilitation and reducing the number of falls. By immersing participants in real life scenarios and monitoring how they their way around obstacles, such as those performed on the GaitBetter system, participants and therapists feel safe and confident while improving motor-cognitive functions over time.
Virtual reality systems can simulate a wide variety of scenarios while keeping safety in check. For those of us who prefer a safe environment without risks, a Virtual Reality simulated hike is the next best thing, as the brain treats it as if it were the real thing.
GaitBetter is a virtual reality motor-cognitive training platform that promotes independence. By engaging participants in interactive cognitive-motor training activities in VR, immersive training can increase the patient’s self confidence while walking, and improve overall quality of life.
To find out more about why you must implement VR in your physical therapy and rehabilitation practice, schedule a meeting with GaitBetter now! Click Here.
